EDIT, March 29, 2016: In addition to having state-run exchanges, there’s another factor involved here, which is much more likely to be the correct explanation. California, Colorado, Connecticut, and Kentucky are the four states that have taken regulatory action to prevent health insurance carriers from cutting commissions. Although my initial hypothesis wasn’t bad, direct action… Read more about Commission cuts aren’t the same in states with state-run exchanges
Humana
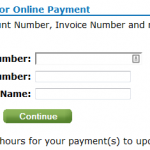
Carrier Contact Information And Updates For People Who Need To Pay January’s Premium
Today, January 10th, is the payment deadline for most Connect for Health Colorado policies with January 1 effective dates. A few carriers have pushed the deadline out a little bit: Updated Anthem Blue Cross and Blue Shield is moving the payment deadline to 1/31 for 1/1 effective dates. Delta Dental: January 15. Premier Access Dental… Read more about Carrier Contact Information And Updates For People Who Need To Pay January’s Premium
Updates For Colorado Residents Enrolling In Exchange Plans After December 23
Connect for Health Colorado is one of only five exchanges that extended the enrollment deadline for a January 1 effective date out beyond Christmas Eve. If you’re in Colorado, you have until the end of the day today (December 27) to enroll in a plan and get a January 1 start date. If you enroll… Read more about Updates For Colorado Residents Enrolling In Exchange Plans After December 23
How Does Obama’s Policy Continuation Announcement Impact Colorado’s Individual Market?
By now you’ve probably heard about the Obama Administration’s compromise over the policy cancellation uproar. The fix that Obama has offered is that health insurance companies can extend existing plans for one more year, allowing them to continue to exist in 2014. This has been incorrectly reported in some media outlets as allowing carriers to continue… Read more about How Does Obama’s Policy Continuation Announcement Impact Colorado’s Individual Market?
Fewer Plans Available In Exchanges In 2013, But Maybe That’s A Good Thing
At the end of September, just as the exchanges were about to open for business, HealthPocket created a comparison of the number of individual and family health insurance policies available in each state in 2013 and compared that with the number of policies that would be available in each state’s exchange in 2014. It’s an… Read more about Fewer Plans Available In Exchanges In 2013, But Maybe That’s A Good Thing
Renewal Options for Each Individual Health Insurance Carrier in Colorado
Last week I explained how early renewal at the end of 2013 might be a good option for some people who have individual health insurance. If you’re happy with your coverage and aren’t going to qualify for a subsidy in the Colorado exchange, keeping your existing plan for most of 2014 might be a good way to save some money on premiums. This is especially true for people who prefer very high deductibles, as those plans are generally not ACA compliant and thus will not be available for purchase after the end of 2013. But if your carrier allows it, you can keep your current policy until it renews in 2014, and switch to an ACA compliant plan at that time. For people with plans that renew late in the year, this could mean keeping a lower-cost, higher deductible policy for most of 2014. If you’ll be eligible for a premium subsidy, it’s definitely worth your time to compare a subsidized exchange plan with what you have now. But if you’re happy with your coverage and you’re going to be paying full price for an ACA compliant plan, check with your carrier to see about keeping your current plan in 2014.
Keep in mind that each Colorado health insurance carrier is doing things a little differently in terms of 2013 renewals heading into 2014. It’s important to check with your carrier to make sure you’re aware of what steps you need to take – don’t assume that  your plan will automatically renew – or automatically not renew. The Colorado Division of Insurance has left a lot of leeway for carriers to determine their own protocol for renewals going into 2014. There is no state requirement that existing policies be cancelled as of the end of 2013, although some carriers have opted for that as a default. All plans must be ACA-compliant by January 1, 2015. So when your policy renews in 2014, you will have to transition to an ACA compliant plan. But the date of that renewal can be anytime from January to December.
your plan will automatically renew – or automatically not renew. The Colorado Division of Insurance has left a lot of leeway for carriers to determine their own protocol for renewals going into 2014. There is no state requirement that existing policies be cancelled as of the end of 2013, although some carriers have opted for that as a default. All plans must be ACA-compliant by January 1, 2015. So when your policy renews in 2014, you will have to transition to an ACA compliant plan. But the date of that renewal can be anytime from January to December.
Here’s a brief summary of what we have heard so far from some of the main carriers in Colorado. This is subject to change, so check with us or your carrier before you make a decision.
Anthem Blue Cross Blue Shield: The default is for your plan to just keep its current renewal date and continue unchanged until that date in 2014. But Anthem is also offering insureds an option […]
Early Renewal Provides A Good Alternative For 2014
Over the last few years, opponents of health care reform have often exaggerated – and sometime outright lied about – the potential negative aspects of the reform law. This has resulted in a public that is often woefully misinformed about what the law does and does not do. But the spin is not limited to just opponents of the law. Sometimes ACA supporters spin things too. This Huffington Post article from a few months ago is a good example. The title, “Aetna seeks to avoid Obamacare rules next year” is designed to play on the general unpopularity (and over-estimation of perceived profits) of insurance companies. When you read a little further, you find that Aetna is reaching out to brokers and insureds to let them know that Aetna will be allowing members to opt for an early renewal in December of this year – if they want to keep their current policy until December 2014.
Why is this being portrayed as a bad thing?
It is indisputable that people who are healthy, buy their own health insurance, won’t qualify for subsidies and prefer high deductible health plans are going to have higher premiums for ACA-compliant plans than they have now. Some of these people don’t mind high deductibles. They don’t consider their policy to be skimpy or junk insurance just because it isn’t ACA compliant. You might have seen headlines about how only a tiny fraction of existing individual health plans meet the requirements that the ACA will impose next year, but that doesn’t mean that the existing  plans are junk. If you look closely, you’ll see that when it comes to basic medical benefits, a lot of individual plans offer coverage that is in line with ACA regulations. But benefits like dental and vision coverage for children (required on ACA-compliant plans starting next year) are usually not part of individual coverage (Many plans allow applicants to select add-on dental and vision coverage, but a lot of people find that it’s more cost effective to pay for dental and vision out of pocket rather than paying for dental/vision insurance. Remember, nothing is free. And the more likely you are to use an aspect of your coverage, the higher your premiums will be in order to cover the cost. So coverage for something like dental and vision checkups – which people plan to use – has to be priced accordingly). In many states, maternity coverage is one of the most significant medical benefits missing from a lot of individual plans. But in Colorado we’ve had maternity on all plans for more than two years now.
plans are junk. If you look closely, you’ll see that when it comes to basic medical benefits, a lot of individual plans offer coverage that is in line with ACA regulations. But benefits like dental and vision coverage for children (required on ACA-compliant plans starting next year) are usually not part of individual coverage (Many plans allow applicants to select add-on dental and vision coverage, but a lot of people find that it’s more cost effective to pay for dental and vision out of pocket rather than paying for dental/vision insurance. Remember, nothing is free. And the more likely you are to use an aspect of your coverage, the higher your premiums will be in order to cover the cost. So coverage for something like dental and vision checkups – which people plan to use – has to be priced accordingly). In many states, maternity coverage is one of the most significant medical benefits missing from a lot of individual plans. But in Colorado we’ve had maternity on all plans for more than two years now.
There are absolutely some bad health insurance plans on the market, with skimpy coverage, limited networks and lots of fine print. But there are also lots of good quality health insurance plans and reputable carriers. And there are plenty of people who are not going to qualify for subsidies next year (roughly half of the people who currently buy individual health insurance). If those people currently have – and are happy with – a high deductible plan that is less expensive than what they would have to pay for an ACA-compliant plan, there’s no reason that they shouldn’t be able to keep their plan as long as possible in 2014. The law requires coverage to be ACA-compliant when a policy renews in 2014. Carriers that are offering early renewals in December are providing good customer service, especially for insureds who […]
Colorado Health Insurance Options On the Exchange in 2014
Although we’re still at least a week away from knowing the specific details on rates and plan designs for policies that will be sold in the Connect for Health Colorado exchange, the Division of Insurance has approved 242 plans that will be available in the exchange from 13 Colorado health insurance carriers. In late May, the number of carriers stood at 11 and the number of plans was 250+. But as we noted last week, there was still a lot going on behind the scenes over the summer, and some carriers had to resubmit plan information that was not accepted in the spring. The final count is 150 plans that will be available to individuals and 92 for small groups (keep in mind that this is just for plans within the exchange. There will be lots of other ACA-compliant plans available outside the exchange).
The plans for individuals will be available from ten different carriers (All Savers, Cigna, Colorado Choice, Colorado Health Insurance Cooperative,  Denver Health Medical Plan, HMO Colorado (Anthem), Humana, Kaiser, New Health Ventures and Rocky Mountain HMO). Although there are some new names in this list, there are also plenty of familiar ones (All Savers is a UnitedHealth company, which means that the main carriers that currently sell policies in the individual market in Colorado will all be represented in the exchange). Although we haven’t yet seen the final premium and plan details, it appears that Colorado will continue to have a robust individual health insurance market in 2014, both in and out of the exchange.
Denver Health Medical Plan, HMO Colorado (Anthem), Humana, Kaiser, New Health Ventures and Rocky Mountain HMO). Although there are some new names in this list, there are also plenty of familiar ones (All Savers is a UnitedHealth company, which means that the main carriers that currently sell policies in the individual market in Colorado will all be represented in the exchange). Although we haven’t yet seen the final premium and plan details, it appears that Colorado will continue to have a robust individual health insurance market in 2014, both in and out of the exchange.
For consumers who will qualify for a subsidy, the exchange is definitely the place to be – subsidies are only available in the exchange. Consumers who do not qualify for a subsidy (either because their income is too high or because they have access to an employer group plan that is technically “affordable” but might actually be outside of their budget) can shop within the exchange (via an approved broker or directly through the exchange) or they can […]
Comparing CEO Compensation in Various Healthcare Industries
Joe Paduda of Managed Care Matters did an excellent job with the most recent Health Wonk Review – be sure to stop by his blog and check it out. I thought this article from Dr. Roy Poses was especially interesting. Writing at Health Care Renewal, Dr. Poses shines the spotlight on UnitedHealth Group’s CEO Stephen Hemsley’s oversized compensation. Roy notes that while the increase in CEO compensation does mirror the company’s overall financial success of late, it must also be considered in light of the fact that the company has made some missteps in terms of fulfilling its stated mission to provide health care “at an affordable price” and “expand access to quality health care.” Roy’s article cites several examples of allegedly unethical behavior, and concludes by noting that “Real health care reform needs to make health care leaders accountable, and especially accountable for the bad behavior that helped make them rich.”
 I definitely do not disagree with Dr. Poses, and we’ve noted in the past that UnitedHealth Group has had issues with large executive compensation and backdating stock options (that was with a previous CEO, however). But I do want to use this as an opportunity to remind our readers and clients that most health insurance companies have CEO compensation packages that are far lower. Forbes compiled a list of the 498 highest-paid CEOs in 2012, and I scrolled through the first 150 on the list. UnitedHealth Group is there on the first page, ranked number 8 (they’re also ranked number 31 in Fortune 500 total profits, so as Roy said, the CEO salary is at least in the same ballpark with the company’s financial performance).
I definitely do not disagree with Dr. Poses, and we’ve noted in the past that UnitedHealth Group has had issues with large executive compensation and backdating stock options (that was with a previous CEO, however). But I do want to use this as an opportunity to remind our readers and clients that most health insurance companies have CEO compensation packages that are far lower. Forbes compiled a list of the 498 highest-paid CEOs in 2012, and I scrolled through the first 150 on the list. UnitedHealth Group is there on the first page, ranked number 8 (they’re also ranked number 31 in Fortune 500 total profits, so as Roy said, the CEO salary is at least in the same ballpark with the company’s financial performance).
But you have to click through several pages of the CEO compensation list to get to the next health insurance carrier. Humana was the next one I found, ranked at […]
Balance Billing From Non-Network Providers Who Work At In-Network Facilities
We recently heard from one of our clients who is dealing with a balance billing issue resulting from a NICU stay. For her baby’s birth, she chose a large hospital in Denver that was on her Humana health insurance network. Her OB/GYN was also on the Humana plan, and she figured she had all of her ducks in a row. But complications necessitated an emergency transfer to the NICU, where her new baby was cared for by doctors who are contracted with the hospital, but are not part of the Humana network.
When patients are treated by out-of network providers, there’s no contractual obligation between the doctors and the health insurance carrier. The patient will usually be responsible for a higher deductible when using a non-network provider (although this is not typically enforced for  emergency care), but even after the deductible is met, the provider is not obligated to accept the “reasonable and customary” payment from the health insurance carrier. The provider can choose to bill the patient the shortfall between what was originally billed and what was paid by insurance.
emergency care), but even after the deductible is met, the provider is not obligated to accept the “reasonable and customary” payment from the health insurance carrier. The provider can choose to bill the patient the shortfall between what was originally billed and what was paid by insurance.
Our client has been balance billed over $5,000 by the NICU doctors. Humana paid the doctors their in-network amounts for the NICU stay and counted it as an in-network expense (ie, no additional out-of-network deductible was charged) because it was an emergency situation. But the doctors refused to accept the insurance reimbursement as payment in full, and billed the family for an additional $5,000+. I suppose it could be worse – this family ended up with a $50,000 balance bill from their baby’s NICU stay.
But it could also be better. People who are recovering from an illness or injury don’t need to also be finding out that an in-network facility where they were treated also has providers who are not […]
Let Medicare Negotiate Drug Prices And The Government Can Afford Subsidies
 Right in the middle of the sequestration mess seems like a good time to discuss the subsidies that are going to be a major part of the ACA starting next year. As of 2014, nearly everyone in the US will be required to have health insurance, and all individual health insurance will become guaranteed issue. There are concerns that premiums in the individual market might increase significantly, but for many families the subsidies enacted by the ACA will help to make coverage more affordable. The subsidies will be available to families earning up to 400% of the federal poverty level; the premium assistance will be awarded on a sliding scale, with the families on the upper edge of that income threshold receiving the smallest subsidies.
Right in the middle of the sequestration mess seems like a good time to discuss the subsidies that are going to be a major part of the ACA starting next year. As of 2014, nearly everyone in the US will be required to have health insurance, and all individual health insurance will become guaranteed issue. There are concerns that premiums in the individual market might increase significantly, but for many families the subsidies enacted by the ACA will help to make coverage more affordable. The subsidies will be available to families earning up to 400% of the federal poverty level; the premium assistance will be awarded on a sliding scale, with the families on the upper edge of that income threshold receiving the smallest subsidies.
But how much will those subsidies cost the taxpayers? How will a government that is so cash-strapped that it’s curbing spending on programs like Head Start and special education be able to fund the subsidies called for in the ACA?
Last summer, the CBO estimated that the exchange subsidies will cost $1,017 billion over the next ten years. Undoubtedly a large sum, but probably necessary in order to make guaranteed issue health insurance affordable for low- and middle-income families.
That sum is partially offset by the CBO’s projections of $515 billion (over the next ten years) in revenue from individual mandate penalties (fines imposed on non-exempt people who opt to go without health insurance starting in 2014), excise tax on “Cadillac” group health insurance policies, and “other budgetary effects” enacted by the healthcare reform law.
That leaves us with $502 billion. Not an insignificant sum of money even when […]
Individual Health Insurance After Donating A Kidney
This recent AARP article caught my attention last week. My father lost his kidneys in 2001 as a result of Wegener’s Granulomatosis, a rare autoimmune disease. In August, he was the recipient of a kidney generously donated by the family of a young man who had passed away. And this fall, for the first time in 11 years, he’s been able to go about his life without being tethered to a dialysis machine every evening. So I’m drawn to stories about kidney transplants, living donors, or families who choose to donate a deceased loved ones organs.
To sum it up, Radburn Royer is a healthy 57 year old who donated a kidney to his daughter four year ago, after her own had failed as a result of lupus. Prior to donating a kidney, Royer was covered by Blue Cross Blue Shield of Minn. It’s unclear what his health insurance status was in the interim, but last year he reapplied for coverage with them and  was turned down. He’s appealed several times, but for now he’s covered by his state’s high risk pool (he has to pay $130 more per month for his coverage and has a higher deductible, both of which are common in high risk pools).
was turned down. He’s appealed several times, but for now he’s covered by his state’s high risk pool (he has to pay $130 more per month for his coverage and has a higher deductible, both of which are common in high risk pools).
Individual health insurance in Colorado is underwritten just as it is in Minn., but underwriting guidelines usually vary from one state to another and from one carrier to another. So we contacted three of the top individual health insurance carriers in Colorado to see how they would underwrite an applicant who had previously donated a kidney. Cigna, Humana and Anthem Blue Cross Blue Shield all said that as long as the donor had been released from medical care and had normal blood pressure and blood lab results, the most likely underwriting outcome would be acceptance with a standard rate.
At first glance, this seems to be at odds with the situation experienced by Royer, but maybe it’s not. The AARP article notes that Royer underwent […]
[…] In the context of kidney donation, it’s important that potential donors not be inadvertently scared off by AARP’s article. Kidney donors are heroes – anyone who had received a transplant will attest to that fact – and they save lives. The study that I linked to above followed donors for 20 – 37 years after their transplants. While some donors did end up having kidney problems, the majority had normal kidney function 20 – 37 years out from surgery, and would likely not have a problem obtaining individual health insurance, even prior to it being guaranteed issue in 2014. Most people who are healthy enough to be accepted as a donor will continue to be healthy after they donate a kidney.
No 2013 CoverColorado Assessment
CoverColorado announced that there will be no assessment in 2013 on Colorado health insurance carriers. The 2012 assessment was roughly $3.79/month/contract for individual/family insureds.
Anthem Blue Cross of Colorado has also announced that their membership this year was higher than expected this year. They were making up for a shortfall by charging $4.36/month/contract in 2012. Due to the higher enrollment, Anthem BCBS has enough funding to satisfy December without billing subscribers a CoverColorado assessment.
Primary Care Practices In Colorado Chosen As Part Of CMS Pilot Program
The Centers for Medicare & Medicaid Services (CMS) announced this week the start of a pilot program to enhance primary care via collaboration among CMS, private health insurance carriers and 500 primary care practices in seven regions across the US. 73 of those practices are in Colorado, with 335 participating physicians, and several of the top health insurance carriers in Colorado are participating too: Anthem Blue Cross Blue Shield, Cigna, Humana, Rocky Mountain Health Plans, and United Healthcare, in addition to Colorado Medicaid, Colorado Choice Health Plans, and Colorado Access (a health plan specifically designed for underserved populations).
CMS will be paying participating providers a “care management fee” which is estimated to be about $20 per month per beneficiary, in addition to the usual fee-for-service reimbursements. The private health insurance carriers that are participating have worked out their own reimbursement schedules, but one would assume that the setup will be similar to the one that CMS has devised. […]
Aetna, Humana and UnitedHealth Vow To Maintain Some Aspects Of ACA, Regardless Of Court Decision
Much of the healthcare community is eager to hear what the Supreme Court has to say – likely next week – about the ACA. Given how polarized the topic of healthcare reform has been over the past few years, there’s no way that any decision is going to please more than about half of the country, although the court has the option of picking and choosing various parts of the law to uphold or overturn as it sees fit.
Some aspects of the ACA have already been implemented and have proven to be very popular. A few of the country’s biggest health insurance carriers have stated that they will keep some of the most popular ACA provisions – even if the law is overturned. Aetna, Humana, and UnitedHealth have said that they will continue to offer preventive care with no cost-sharing, allow young adults to remain on their parents’ health insurance policy through age 26, and maintain the third-party appeals process that insureds can use if a claim is denied. Humana and UnitedHealth have also said that they will continue to have no lifetime benefit maximums on their policies and ban rescission except in cases of fraud. […]
Best Health Insurance Companies In Colorado
We recently got a call from a client who mentioned that he had done a Google search for the “best health insurance companies in Colorado” and his concern was that Anthem Blue Cross Blue Shield was not on the top ten list that he said came up as the first search result. We were a… Read more about Best Health Insurance Companies In Colorado
Would Premiums Without A Mandate Really Only Be 2.4% Higher Than With A Mandate?
[…] Keep in mind that all of those prices are based on the fact that the individual policies are medically underwritten (which means that the rates can be increased during underwriting or the application can be denied based on medical history), while the group plans are guaranteed issue and the rates cannot vary based on the group’s health status. There’s a huge range of options available, both in the individual and small group markets. But the premiums in the small group market for our family of four (parents in their 30s with two young children) would be roughly double what they are in the individual market.
Although I realize that the RAND study is important and useful, I wonder why the real-life scenario of individual versus small group premiums is so different. And although the ACA does put a cap on how much greater premiums can be for older people versus younger people, it doesn’t stipulate what the base premiums have to be for the younger people. Premiums have to follow the MLR rules (with insurers spending at least 80 – 85% of premiums on medical expenses), but they will reflect claims expenses pretty closely. […]
Colorado Child-Only Open Enrollment Details For January 2012
The next open enrollment for child-only policies is almost here, so I thought it might be helpful to provide some specific details in terms of what policies are available and what parents should expect when submitting child-only applications next month.
The first open enrollment window in 2012 will be the month of January. Applications for child-only policies have to be submitted between January 1 and January 31. Application not submitted by the end of January will have to wait and re-submit in July, which is the second open-enrollment period of the year. For most carriers, each child in a family will have to have a separate application.
All eligible child-only applications submitted during the open enrollment period are guaranteed issue, so the child cannot be refused coverage. However, the applications are still medically underwritten and the rate can be increased by up to 200% based on the child’s medical history (so if the standard price is $100, the policy could actually be assigned a rate of $300, which is equal to a 200% rate increase).
Colorado Senate Bill 128 requires all Colorado health insurance carriers that offer coverage for adults to also offer child-only plans during the two annual open enrollment windows. But the bill does not require carriers to provide guaranteed issue coverage for children who are eligible for health insurance from another source (other than a high risk pool like CoverColorado or GettingUSCovered – see the bottom of page 4).
Most Colorado carriers have selected one or two plan designs that will be available for child-only applications next month. To give you an idea of what is available in Colorado for child-only coverage, we’re providing information here regarding child-only options from six of the top individual health insurance carriers in the state. […]
Employer Funding of Individual Health Insurance – The Rules Are Changing
[…] Because of the new law, employers can now use wage adjustments to reimburse employees for individual policies (as long as they haven’t had a group policy in the past twelve months), which wasn’t allowed at all in the past. But the use of HRAs to fund individual policies can now only be done if the employer hasn’t had a group policy in the past twelve months, and that restriction wasn’t found in the DOI final agency order regarding HRAs. […]
Rate Review Process Does Not Keep Premiums Artificially Low
[…] If the rates are justified, they’ll likely be approved – even if the amount of the increase is distastefully large. The DOI is not trying to keep premiums artificially low or force carriers to cut out legitimate claims expenses. Having rates approved by the DOI does not mean that the people of Colorado get smaller-than-average premium increases. Rather, it means that although our rate increases are sometimes substantial, we know that those rates are justified as a reflection of increasing claims costs.
Humana 2011 Rates Are Official
Clients in Colorado can now get quotes and apply for HumanaOne with effective dates of 1/1/2011 or later. Remember, these will include maternity coverage as a base benefit. Existing members with an Enhanced, Copay, HSA, or Value plan will receive these benefit changes at the time of their renewal. For clients who have an Autograph,… Read more about Humana 2011 Rates Are Official
Maternity Coverage In The Individual Health Insurance Market
The House Committee on Energy and Commerce released a memorandum this week detailing the practices of the four largest private health insurance carriers (Aetna, Humana, UnitedHealth Group and Wellpoint) regarding maternity coverage on individual policies. For anyone who is familiar with the individual health insurance market, the details of the memo will come as no surprise. But since the majority of Americans are covered by group health insurance plans that cover maternity just like any other claim, the details of how maternity coverage works in the individual market may be eye-opening for a lot of people. […]
Regulators And Insurers Still Working On Child-Only Coverage Issue
[…] So far, none of the carriers who had backed out of the child-only market have commented on whether the open enrollment periods might make them change their minds, but AHIP (America’s Health Insurance Plans) has said that they are continuing to work with regulators to try to find solutions that would make the child-only market feasible for insurers in the future.
Quoting Blackout On Most Plans and Effective Dates
Many plans with most carriers still haven’t gotten the rates approved past 9/23. These plans with carriers like Anthem BCBS can still be quoted with effective dates of 9/22 and before.
Carriers like Cigna only have 1st and 15th of the month effective date options. Therefore, rates and plans are not being quoted at all until the DOI approves their rates. Hopefully any moment.
Make sure to subscribe via email or follow us on Facebook for rate approval updates.
Guaranteed Issue Policies For Children Happened Too Quickly
[…] Regardless of the practicalities involved, there’s no doubt that the headlines about insurers ceasing to issue child-only policies is generating some ill will and bad PR for insurance carriers. Either lawmakers knew that would happen, or else they put very little thought into considering the details of how insurers would go about making children’s coverage guaranteed issue a mere six months after the bill was signed into law, and just added the provision as a feel-good part of the bill.