David Williams hosted a great Health Wonk Review this week, and it was interesting to see how he divided the articles into optimistic and pessimistic viewpoints, with one section for “glass half full” articles, and another for the “glass half empty” ones. It’s a reminder that there are always different ways of looking at the… Read more about Our Glass Is Half Full And We Like It That Way
Blog
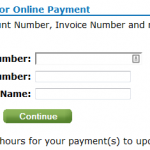
Carrier Contact Information And Updates For People Who Need To Pay January’s Premium
Today, January 10th, is the payment deadline for most Connect for Health Colorado policies with January 1 effective dates. A few carriers have pushed the deadline out a little bit: Updated Anthem Blue Cross and Blue Shield is moving the payment deadline to 1/31 for 1/1 effective dates. Delta Dental: January 15. Premier Access Dental… Read more about Carrier Contact Information And Updates For People Who Need To Pay January’s Premium
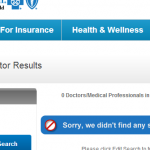
Do Not Assume Your Provider Network Will Be The Same As It Was Last Year
A description of PPO, HMO, EPO and a search tools for all carriers is available here. EDIT 2/18/14: Connect for Health Colorado updates the provider directory once per month. It is possible therefore that the list may not be up-to-date at all times. If you have questions, you can call your carrier directly, or contact… Read more about Do Not Assume Your Provider Network Will Be The Same As It Was Last Year
Kicking Off 2014 With A Great Risk Round Up
Michael Stack from Workers’ Comp Resource Center hosted the first Cavalcade of Risk for 2014, full of lots of good risk-related articles. If you’re looking for a really interesting read, I recommend David Williams’ post about medical child abuse and a case that has pitted Boston’s Children’s hospital against a patient’s parents. David links to… Read more about Kicking Off 2014 With A Great Risk Round Up
Updates For Colorado Residents Enrolling In Exchange Plans After December 23
Connect for Health Colorado is one of only five exchanges that extended the enrollment deadline for a January 1 effective date out beyond Christmas Eve. If you’re in Colorado, you have until the end of the day today (December 27) to enroll in a plan and get a January 1 start date. If you enroll… Read more about Updates For Colorado Residents Enrolling In Exchange Plans After December 23
Dear Santa: Can you help me pick my favorite entry in a stellar HWR?
Julie Ferguson hosted one of the best ever Health Wonk Reviews yesterday at Workers’ Comp Insider. Definitely something for everyone – and lots of holiday cheer – in this “Dear Santa” edition. I had so many favorites that I couldn’t narrow it down to just one or two, so here are my votes for the… Read more about Dear Santa: Can you help me pick my favorite entry in a stellar HWR?
What Is An Essential Health Benefit (EHB)?
Essential Health Benefits (EHBs) are one of the most important aspects of the ACA’s transformation of the individual health insurance market (they also apply in the small group market, but group policies have historically been more benefit-rich than plans sold in the individual market). In the past, insurers were given tremendous leeway in plan design;… Read more about What Is An Essential Health Benefit (EHB)?
Pediatric Dental on 2014 Individual Health Insurance Policies in Colorado
If you’re confused by the new pediatric dental requirements, you’re not alone. Here’s a rundown of how the ACA and HHS regulations impact pediatric dental coverage, with Colorado-specific details: The ACA defines pediatric dental coverage as one of the ten essential health benefits (EHBs) that must be covered on all new individual and small group… Read more about Pediatric Dental on 2014 Individual Health Insurance Policies in Colorado
The Cavalcade of Risk – making us all smarter since 2006
Be sure to check out the latest Cavalcade of Risk, hosted by David Williams. For all of us who love a nurse, Julie Ferguson’s post from Workers’ Comp Insider is an eye-opener… not only do nurses face on-the-job violence and abuse from patients, but also from other staff members. And Mom and Dad Money has… Read more about The Cavalcade of Risk – making us all smarter since 2006
Good News From the Health Wonks for ACA Enrollment in 2014
Jason Shafrin hosted the latest Health Wonk Review at The Healthcare Economist, and it’s an excellent edition. It’s mostly all about the ACA, and there are lots of different viewpoints to consider. One of my favorite posts in the HWR is from Health Affairs, written by Rick Curtis and John Graves. Rick and John make… Read more about Good News From the Health Wonks for ACA Enrollment in 2014
Tobacco Use: ACA and Colorado Regulations
Back in January, I looked at the issue of tobacco use and the ACA from a mostly philosophical perspective. But we also wanted to provide a summary of what’s going on here in Colorado with regards to tobacco and the new health insurance policies that are available for 2014. Although the ACA has eliminated the practice of… Read more about Tobacco Use: ACA and Colorado Regulations
Catastrophic Plans Not Significantly Less Expensive In Colorado
Even if you’ve been paying pretty close attention to media coverage of the ACA over the last few years, you might not know a whole lot about the ACA’s catastrophic plans. They haven’t been heavily publicized by HHS or the rest of the Obama Administration, they’re not eligible for subsidies, and they have relatively thin… Read more about Catastrophic Plans Not Significantly Less Expensive In Colorado
Thanksgiving Cavalcade of Risk
Happy Thanksgiving and welcome to the 197th Cavalcade of Risk! If you’re a brave soul who relishes the thought of a family dinner filled with spirited debates about healthcare reform, insurance and risk, we’ve got plenty of fodder for your conversations. Just don’t steer the conversation over the line into politics, especially after a glass… Read more about Thanksgiving Cavalcade of Risk
Imagine How Much Better Open Enrollment Would Have Been Without The Exchanges
We’ve all heard Secretary Sebelius talk about how amazing it is that “for the first time” Americans who buy their own health insurance have a place where they can see all of their options in one place, compare plans, and enroll in coverage. Anyone who has taken more than a cursory glance at the individual health… Read more about Imagine How Much Better Open Enrollment Would Have Been Without The Exchanges
Rational Thoughts on the Exchange Rollout, and Other Health Wonkery
Hank Stern did an excellent job hosting the Health Wonk Review today. Head over to check it out – you’ll learn all sorts of things about health care policy and reform, and you’ll also learn why this Thanksgiving/Chanukah overlap is truly a once in a lifetime event. My favorite posts in this edition come from… Read more about Rational Thoughts on the Exchange Rollout, and Other Health Wonkery
How Does Obama’s Policy Continuation Announcement Impact Colorado’s Individual Market?
By now you’ve probably heard about the Obama Administration’s compromise over the policy cancellation uproar. The fix that Obama has offered is that health insurance companies can extend existing plans for one more year, allowing them to continue to exist in 2014. This has been incorrectly reported in some media outlets as allowing carriers to continue… Read more about How Does Obama’s Policy Continuation Announcement Impact Colorado’s Individual Market?
Colorado Senator Udall Introduces Bill To Allow Individual Policies To Continue For Two More Years
Colorado Senator Mark Udall introduced legislation today that would allow people with individual health insurance to keep their existing policies for two more years – through the end of 2015 – regardless of any cancellation notices that have already been sent out. Udall’s Continuous Coverage Act is designed to smooth the transition to ACA-compliant plans…. Read more about Colorado Senator Udall Introduces Bill To Allow Individual Policies To Continue For Two More Years
News From The Health Wonks – Lots Going On In Health Care Reform Land
Brad Wright did an outstanding job with the Health Wonk Review this week, hosted at his always excellent blog, Wright on Health. There are plenty of posts about the latest in ACA implementation, including several differing viewpoints on the recent news about policy cancellations. I particularly liked Joe Paduda’s article about Medicaid expansion – it’s an… Read more about News From The Health Wonks – Lots Going On In Health Care Reform Land
Getting Past The Health Insurance Plan Cancellation Hysteria
Much has been said recently about how the ACA is causing a tidal wave of policy cancellations, and resulting in people losing coverage that they would prefer to keep. The frustrating part about this – as has generally been the case with every big uproar about the ACA – is that we’re not really getting… Read more about Getting Past The Health Insurance Plan Cancellation Hysteria
Fewer Plans Available In Exchanges In 2013, But Maybe That’s A Good Thing
At the end of September, just as the exchanges were about to open for business, HealthPocket created a comparison of the number of individual and family health insurance policies available in each state in 2013 and compared that with the number of policies that would be available in each state’s exchange in 2014. It’s an… Read more about Fewer Plans Available In Exchanges In 2013, But Maybe That’s A Good Thing
The Public Should Be Aware Of Actual Health Insurance Premiums As Well As Subsidized Rates
Jaan Sidorov hosted this week’s Health Wonk Review at his most excellent Disease Management Care Blog – be sure to check it out if you haven’t already. One particularly interesting post in this edition comes from Hank Stern, writing about how one of the widely-criticized flaws in the HHS-run exchanges was actually an intentional part… Read more about The Public Should Be Aware Of Actual Health Insurance Premiums As Well As Subsidized Rates
Early Renewal Does Not Mean You’re Taking Advantage of a Loophole
A few weeks ago, I wrote a post about our family’s health insurance policy and the changes coming in 2014. To make a long story short, our premiums are going to go up significantly and we don’t qualify for subsidies. We’re not complaining… we know that the ACA makes healthcare more accessible for a lot… Read more about Early Renewal Does Not Mean You’re Taking Advantage of a Loophole
The Government May Be Shut Down, But the Health Wonk Review Is Open For Business
Joe Paduda did an outstanding job with the most recent Health Wonk Review, hosted at Managed Care Matters. This edition is all about the government shutdown and Obamacare, and there’s a little something for everyone. My favorite article in this HWR comes from David Williams, explaining why Conservative lawmakers ostensibly hate Obamacare – along with… Read more about The Government May Be Shut Down, But the Health Wonk Review Is Open For Business
House Republicans Want To Strip Congressional Staffers Of Their Health Insurance Benefits
Yesterday I explained why the Republican House Amendment to “delay Obamacare” (actually, just the individual mandate) would be impossible from a practical standpoint. I am not under any illusions that the people who created it were actually trying to implement something practical or realistic. They don’t care that millions of people have been waiting 3.5 years since the ACA became law to be able to enroll in guaranteed issue individual health insurance. They don’t care that millions of uninsured Americans will finally be able to afford health to purchase their own health insurance thanks to the subsidies in the marketplaces/exchanges. Their priority is to get rid of the ACA, and it appears that they consider the shutdown of the federal government to be acceptable collateral damage in their fight. Their goal is not really to delay the law, but to derail it entirely – they know full well that delaying the individual mandate would throw the whole law into a tailspin.
But there’s another part of the House Amendment to H.J. Res. 59 that is also worth talking about, since it goes hand in hand with an ACA myth that just won’t die. So before we go any further, I want to clarify: Congress is not exempt from the ACA. The President and Vice-President are not exempt from the ACA. Political Appointees are not exempt from the ACA. Being “exempt from the ACA” or “exempt from Obamacare” doesn’t really mean anything anyway. The talk show hosts who perpetuate this myth are deliberately trying to obfuscate an aspect of the ACA that actually penalizes Congress.
They talk about how this amendment gets rid of “special treatment” for Congress. If you consider losing your employer-sponsored health  insurance to be “special treatment,” then I guess that’s true. The amendment basically lays out provisions to make sure that the President, Vice President, political appointees, Congress and congressional staffers must purchase health insurance in the marketplaces (exchanges) and strips them of any contributions from the government to help pay for their policies.
insurance to be “special treatment,” then I guess that’s true. The amendment basically lays out provisions to make sure that the President, Vice President, political appointees, Congress and congressional staffers must purchase health insurance in the marketplaces (exchanges) and strips them of any contributions from the government to help pay for their policies.
To briefly summarize the history of this fight, back in 2010 Republican Senator Chuck Grassley felt that “we [in Congress] need to go into the exchange so that we would have to go through the same red tape as every other citizen.” This is sort of a warm-fuzzy statement if you just take it at face value. But in truth, it’s ridiculous, because the majority of US citizens are not going to be using the exchanges. Most people will continue to get their health insurance from their employers or from the government (Medicare, Medicaid, VA).
Federal government employees get their health insurance from the Federal Employees Health Benefits Plan (FEHB). Just like almost every very large employer, the federal government provides health insurance benefits to its workers and pays a large portion of the premiums. The benefits are one of the ways that the government is able to recruit talented employees. The marketplaces/exchanges were created in order to help people who are uninsured or who purchase their own individual health insurance (because they are self employed or work for a company that doesn’t provide benefits). Federal government employees do not fall into this category by any stretch of the imagination. So it has always seemed ridiculous to me that the Grassley Amendment was added in the first place. But it was.
Although the original amendment didn’t include a provision for Congress et al to keep their employer contributions (the amount that the government already pays towards their FEHB policies) and use them towards individual health insurance in the marketplaces, it also did not require the government to stop contributing to their health insurance premiums. The Office of Personnel Management (OPM) issued a proposed ruling in August that allowed the government to continue to fund Congressional health insurance after the switch is made from FEHB to the exchanges. Then at the end of September, OPM issued a final ruling which states that
“OPM has clarified that Members of Congress and designated congressional staff must enroll in an appropriate Small Business Health Options Program (SHOP) as determined by the Director in order to receive a Government contribution.”
This is what they came up with in order to work around an amendment that never made sense in the first place. The OPM ruling doesn’t really make a whole lot of sense either, since the SHOP marketplaces in 2014 are designed for businesses with up to 50 employees – not exactly the definition of the federal government’s employment roster. But the SHOP markeplaces are set up to allow employers to contribute to  their employees’ health insurance premiums, so it works on that level.
their employees’ health insurance premiums, so it works on that level.
And now the House Amendment to H.J. Res. 59 would remove that allowance. It states that “No government contribution under section 8906 of title 5, United States Code, shall be provided on behalf of an individual who is a Member of Congress, congressional staff, the President, Vice President, or a political appointee for coverage under this subparagraph.” The basic effect of this would be to strip these government employees of their employer-sponsored health insurance benefits, even though these benefits are part of what helps keep the government competitive with other big companies in the labor market. Keep in mind that we’re not just talking about highly paid lawmakers… congressional staffers are included. These are regular people with jobs that probably aren’t all that glamorous. And now House Republicans want to strip them of their employer-sponsored health insurance benefits?
Interestingly enough, Senator Grassley has said that he didn’t intend for lawmakers to lose the money that the federal government contributes towards their health insurance coverage (just like any other large employer would). And yet, here we are.
Overall, the House Amendment to H.J. Res. 59 is a mess. It makes no sense, and lawmakers who voted against it should be commended. It’s only seven pages long, so take a look at it yourself if you’re curious. As I mentioned in yesterday’s post, there are much more productive, sensible ways that Speaker Boehner and his colleagues could go about changing the law, if they’re so inclined. They’re throwing a Hail Mary here, because they know that once the marketplaces are running smoothly and people get used to guaranteed issue health insurance and subsidies to help pay for it, the ACA will probably be a pretty popular law. An amendment that attempts to hobble the law under the guise of “delaying” it is disingenuous. The American people deserve better than this.
Government Shutdown: Is The Republican “Plan” Actuarially Feasible?
Although I’ve seen a lot of media references placing blame for the government shutdown squarely at the feet of House Republicans, I’ve also heard people saying that both sides are to blame and that the Democrats could have “compromised.” I’ve just finished reading the text of the House amendment to H.J. Res. 59. This is the amendment that would have “delayed Obamacare” by a year.
There are a couple specific aspects of the ACA that House Republicans were trying to delay or delete. The most significant is the individual mandate (keep in mind that this has been challenged all the way to the Supreme Court and found to be Constitutional), which the amendment would postpone until 2015. [The amendment also contains some other provisions regarding health insurance for Congress and the President, which I’ll address tomorrow.]
The initial provisions of the ACA started to take effect in 2010. January 1, 2014 is about 3.5 years after that, so the individual mandate had a significant built-in delay. But let’s assume for a moment that the Democrats wanted to accept this “compromise” and allow the individual mandate to be delayed until 2015. What would that have involved from a practical standpoint?
An actuarial nightmare
Back in the spring of this year, health insurance carriers all across the country were scrambling to submit rates and plan designs for review. There were some delays, and some carriers ended up having to redo their rates and submit them again, but by the middle of August we had a pretty good idea of what plans were going to be available in the Colorado marketplace (exchange) – and news was also coming in from lots of other states. This was six weeks before the marketplaces opened, and a full 4.5 months before the new policies were going to be effective. Once the rates were finalized, they had to be loaded into each marketplace’s online quoting software so that they would be available to navigators, brokers and applicants once the marketplace opened for business.
This whole process took many months. Creating the ACA-compliant plan designs and doing the actuarial work to price them was not something that happened overnight. Carriers were working on this early in the year, getting their plan design and rate info ready to submit in the spring. And then the rate reviews, final approval, and user interface updates added to the time frame.
So let’s go back and look at the Republican “compromise” of delaying the individual mandate for a year. All of the new plans and rates that actuaries, marketplaces and Divisions of Insurance have been working with this year are designed around the basic concepts of the ACA: Policies  must be guaranteed issue (a huge change from the way policies have historically been issued in the individual market, where underwriting has been part of the process in all but five states), they can only be issued during open enrollment or following a qualifying event (loss of other coverage, birth, adoption, marriage, divorce), and the individual mandate is expected to generally increase enrollment.
must be guaranteed issue (a huge change from the way policies have historically been issued in the individual market, where underwriting has been part of the process in all but five states), they can only be issued during open enrollment or following a qualifying event (loss of other coverage, birth, adoption, marriage, divorce), and the individual mandate is expected to generally increase enrollment.
Removing any of these elements would drastically change the pricing of the policies and basically mean that the actuaries would have to start over. Incidentally, the House Amendment does not mention delaying the requirement that individual health insurance be guaranteed issue starting in 2014. To roll out guaranteed issue coverage without the individual mandate would mean that rates would be significantly higher for the people who do opt to purchase a plan. But regardless, removing one of the primary elements upon which the 2014 rates have been based would mean a complete do-over of the actuarial process of pricing the new policies.
But what about just keeping things the way they are? Can’t we just keep our 2013 plans and roll them into 2014 with no changes?
No. Remember, the House Amendment to “delay Obamacare” (that’s the language most often used in the media and by lawmakers themselves) would actually just delay the individual mandate. It doesn’t delay the other crucial aspects of the ACA that guided plan design for 2014. So policies would still have to provide essential health benefits. They would have to be guaranteed issue and priced the same regardless of gender (in Colorado, this has been the rule for almost three years now, but the ACA bans it everywhere).
So current 2013 policies could not continue to be issued in 2014. They’re not compliant in terms of plan design, even if actuaries were able to perform a miracle and redo all of the pricing in the next few weeks.
That puts us back to starting over with the new ACA-compliant plans that carriers created months ago, and trying to reprice them for 2014 to reflect a delay in the individual mandate. Remember that the actuaries have to come up with the pricing (not a quick process), DOIs and marketplaces have to review the pricing, and then the final rates have to be uploaded to quoting systems (both marketplace systems and private “off-exchange” quoting systems) and added to printed sales materials in time for consumers to be able to use them. For 2014 plans, this process started early in 2013. Starting over at the beginning of October would have been mission impossible.
Consumers have generally always been able to submit applications one to two months prior to the effective date they want. A lot of people wait until the last minute, but quotes are available several weeks out. That means that if actuaries were to start over at the beginning of October and redo everything, the entire process would have to be completed by mid November at the latest in order for accurate pricing information to be available for consumers looking for a January 1 effective date. The House Amendment did not mention delaying the opening of the marketplaces, so it’s unclear what lawmakers wanted the marketplaces to do. Would plan information still be available in early October, but with no rate data?
To say that this was a poorly planned amendment is an understatement. It was political posturing designed to appeal only to people who “hate Obamacare” (and unfortunately, some of those people are woefully uninformed about the law). It had no basis in actuarial reality, and would have thrown […]