Connect for Health Colorado is one of only five exchanges that extended the enrollment deadline for a January 1 effective date out beyond Christmas Eve. If you’re in Colorado, you have until the end of the day today (December 27) to enroll in a plan and get a January 1 start date.
If you enroll between December 24 and December 27, your account will show a February 1 start date. The exchange will be changing this manually next week, and your account will be updated to show a January 1 start date.
 Data from Connect for Health Colorado is being transmitted to carriers each day, but it can take up to two days for the enrollment to be available in the carrier’s system. You can contact the carrier regarding your application, but you should wait a couple of days after enrolling so that the carrier has your information when you call.
Data from Connect for Health Colorado is being transmitted to carriers each day, but it can take up to two days for the enrollment to be available in the carrier’s system. You can contact the carrier regarding your application, but you should wait a couple of days after enrolling so that the carrier has your information when you call.
In order to get a January 1 start date, you must pay your first premium by January 10. Be aware that it can take up to 10 days after you enroll before the carrier sends out your invoice. If you’re enrolling on December 27, this could put you very close to the January 10 due date, so it’s vitally important that enrollees keep on top of this. Some carriers are allowing online or phone payments once your enrollment data is in their system. Other carriers need to have your invoice number before they can accept payment. In all cases, you can pay by check once you receive your invoice, but you must be sure that your payment is received by January 10. So if you receive your invoice within just a few days of the deadline, call your carrier to see what course of action they recommend. In many cases, they’ll be able to accept payment over the phone or online, ensuring that your payment is received on time.
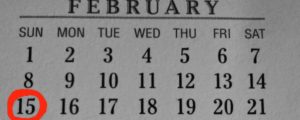
If you enroll with any carrier anytime between December 28 and January 15, you’ll get a February 1 effective date.
HUMANA UPDATE: For anyone who has purchased a new individual Humana plan with a January 1 effective date: Humana will be sending you a member ID card and invoice in the next few weeks. If you have not received your ID card and invoice by mid-January, call Humana at 1-800-223-3659 (or you can call us and we’ll check on it for you). Once you receive your invoice, you can pay your premium at MyHumana.com. Humana is allowing new insureds until January 31 to pay the first premium. You’ll also be able to change your assigned PCP (if applicable) on the MyHumana site. Humana has also notified us that they are processing a backlog of paper applications for off-exchange products. If the application was received by Humana on or before December 23, it will be processed with a retroactive January 1 effective date (it will show in the system initially with a Feb 1 effective date, but this will be changed). If you’re submitting an application now for a February effective date, it’s best to apply online or with Humana’s phone application system – paper applications are likely to result in a delay.