Earlier this month, lawmakers in Florida passed House Bill 221 in an effort to prevent surprise balance billing when patients are treated by out-of-network providers at in-network facilities. Governor Scott hasn’t yet signed HB221 into law, but details about how the law would work are outlined here.
HB221 is being called a model for other states to follow, and heralded as good progress towards protecting patients from balance billing. But I don’t think it goes far enough in terms of consumer protections – even if HB221 is enacted, there will be people caught by surprise balance bills.
How does surprise balance billing happen at in-network hospitals?
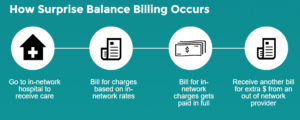 Balance billing happens when a patient sees an out-of-network healthcare provider. The patient’s health insurance may or may not pay some of the charges, but the provider is also able to bill the patient above and beyond what the insurer pays (if anything), as the provider doesn’t have a contract with that patient’s insurer. That contract is what prevents balance billing when you see a provider who is in your insurer’s network – in that case, the provider has agreed to your insurance company’s fee schedule, and must accept it as payment in full.
Balance billing happens when a patient sees an out-of-network healthcare provider. The patient’s health insurance may or may not pay some of the charges, but the provider is also able to bill the patient above and beyond what the insurer pays (if anything), as the provider doesn’t have a contract with that patient’s insurer. That contract is what prevents balance billing when you see a provider who is in your insurer’s network – in that case, the provider has agreed to your insurance company’s fee schedule, and must accept it as payment in full.
Balance billing is fair enough when patients are clearly informed about the network arrangements of their health care providers and choose to go outside of their plan’s network. But it starts to fall apart a bit when patients use an in-network hospital and are treated by doctors at that hospital who aren’t in the same networks as the hospital.
When Jay had knee surgery several years ago, we knew to watch out for this, because we’re in the health insurance industry. We asked about imaging, assistant surgeons, and the anesthesiologist, and were reassured that they were all in-network with our insurance carrier. But we didn’t think to ask about the durable equipment supplier, who turned out to be out-of-network. In our case, it was only a few hundred dollars in extra charges, but some patients end up with balance bills for tens of thousands of dollars – sometimes for treatment that they didn’t even know they received (eg, an assistant surgeon who worked on them while they were under anesthetic; in Jay’s case, the ice machine was already attached to his leg when he woke up, and the crutches had already been delivered to his room).
In Florida, HB221 would require hospitals to post links to all the health insurers with which they’re contracted, along with a list of all the medical providers who provide services in the hospital, and a statement informing patients that those providers may or may not be contracted with the same health insurance carriers as the hospital. Patients would then be advised that they should contact the providers directly to see if they’re in-network, prior to receiving non-emergency care.
Under HB221, balance billing would be prohibited in non-emergency situations if
- The patient is treated at a hospital that is in the patient’s health insurance network
AND
- “the insured does not have the ability and opportunity to choose a participating provider at the facility who is available to treat the insured.”
That second part seems problematic. There’s just too much grey area there. Don’t get me wrong – I love the idea of legislation that would prevent surprise balance billing when patients use in-network hospitals. But it still seems like HB221 puts too much of the onus on the patient to sort out an issue that’s probably beyond the expertise of the average patient. And there’s too much leeway for providers to claim that the patient may actually have had the “ability and opportunity” to pick an in-network provider instead.
Patients might not be aware of the full range of providers they may encounter during their time in the hospital, and may not be in the right frame of mind to be sorting out issues like this. It’s tricky to stop every provider who walks into your room and ask to double check their network affiliations before letting them touch you.
What if we just let hospitals and providers work this out themselves, taking the patient out of the equation altogether?
How about requiring hospitals to only contract with providers who are in the same insurance networks as the hospital? Or in the case of narrower networks where insurance carriers limit the scope of the network in order to gain rate negotiating power, physicians who get privileges at a hospital would have to agree to accept as payment in full whatever the network rates are for the various health insurance carriers with which the hospital contracts.
In Florida, some radiologists and anesthesiologists fought against HB221, and Florida Sen. Rene Garcia (R, Hialeah), who sponsored the Senate’s version of the legislation, noted that those two groups of physicians fought “tooth and nail” to stop HB221. Garcia said the doctors’ efforts to block the legislation were “a clear indication that they want to see this bill killed because they want to continue to balance bill, and they’re the ones who have been the number one abusers.” This makes sense, as radiologists and anesthesiologists tend to be the doctors who come in after the treatment has already begun, or might not even interact with the patient – it’s easy to see how patients could be caught off guard by a bill from a radiologist or anesthesiologist who isn’t in the same network as the hospital.
If hospitals simply required all of their contracted physicians to accept network rates for all of the insurance plans with which the hospital is in-network, the doctors would have to make a choice – accept in-network payment as payment-in-full, or lose privileges at that hospital.
On the flip side, insurance carriers would have to agree to pay all of a hospital’s contracted physicians in-network rates for services performed in order to make this work. For health insurance plans that don’t cover out-of-network care at all, the network agreement with each hospital would have to extend to all physicians who provide care in that hospital.
One way or another, it should not be a patient’s responsibility to ensure that every person who will be providing care at an in-network facility is actually in the network. The fact that we have such a system now is asinine, and adds another layer of complexity to a healthcare system that can often feel overwhelming for patients.


