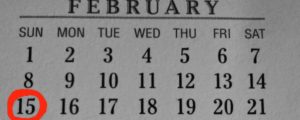
It’s open enrollment time again, and happily, this one is certainly off to a better start than last year. The downside is that there’s only a month between the start of open enrollment and the December 15 enrollment deadline for people who need their new coverage to be effective January 1 (this is the case in Colorado and almost everywhere else, although there are four states with later deadlines). But the good news is that people – lots of them – have been able to enroll in the first  few days of open enrollment, and the drastic technology problems we saw last year aren’t cropping up this year.
few days of open enrollment, and the drastic technology problems we saw last year aren’t cropping up this year.
If you get started on your enrollment soon, you should be able to get everything squared away for a new policy that starts in January, without much in the way of headaches (we’ve put together a list of tips and recommendations – check them out if you’re planning to enroll in a plan in Colorado during this open enrollment).
But with the start of open enrollment, I’m reminded of all the ways I’d like to see the ACA improved. I know the “full repeal” crowd in Congress isn’t likely to sit down with the legislators who drafted the ACA and work on fixes anytime soon, but here’s what’s on my wish list, just in case they’re interested:
- Fix the “family glitch.” First and foremost, this would be my number one request. I wrote about it nearly a year and a half ago, before anyone started enrolling in ACA-compliant plans. It’s still a problem, and it’s something that comes up a lot for us and our clients. Over the years, a significant number of our clients have been in exactly the situation that is so problematic in the family glitch. One person in the household has an employer plan that offers reasonably-priced coverage to the employee. But adding dependents is far too expensive, which is why those people have traditionally turned to the individual market for less-expensive coverage. They can still do that, but if the employee’s cost to cover just the employee on the group plan is less than 9.5% of the household’s income (9.56% in 2015), the dependents are not eligible for subsidies in the exchange, regardless of how expensive it would be to add them to the employer plan. Al Franken – among others – has tried to fix the family glitch, and hopefully lawmakers will successfully resolve this soon. If a family is enrolled in a employer plan, it’s only fair to judge the affordability of that plan based on the cost to cover the whole family. If it’s not affordable, and assuming they meet the rest of the eligibility rules for subsidies in the exchange, they should be able to get subsidies in the exchange.
- Allow copper plans to be added to the mix of coverage options. Copper plans would be policies with higher deductibles and higher out-of-pocket exposure than currently allowed under the ACA. They would have an actuarial value (AV) of 50%, but they would still be solid, ACA-compliant coverage after the out-of-pocket maximum is met. They would have lower premiums than bronze plans, but unlike the current catastrophic plans, they would also be available to anyone who wanted them and premium subsidies could be used to lower the cost of purchasing them. Of course they wouldn’t be a great choice for a lot of people. But for some people, they would be a good fit. As long as we know that the plans are solid, ACA-compliant coverage after the out-of-pocket maximum is met, there’s nothing wrong with allowing people to self-insure all but the catastrophic claims, if that’s their preference.
- Make premium subsidies available below poverty level in states that haven’t expanded Medicaid. This – thankfully – doesn’t apply in Colorado, because Colorado has expanded Medicaid. That means that people here with incomes below 133% of poverty are eligible for Medicaid. That was the way it was supposed to be in every state, but 23 states have not expanded Medicaid, following a Supreme Court decision in 2012 that allowed states to choose whether or not to expand Medicaid. Unfortunately, premium subsidies in the ACA are only available to people with incomes between 100% and 400% of poverty level (remember, this is not a flaw in the ACA as it was written… everyone below 100% of poverty level was supposed to have Medicaid). There’s growing pressure in those 23 states to expand Medicaid, and I think they eventually will. But it could easily be five to ten years before that happens in some states. And in the meantime, there are 3.8 million people in those states who have no realistic access to health insurance at all. They don’t qualify for Medicaid, and they can’t get premium subsidies either. They can’t afford to pay full price for coverage when they live below the poverty level ($19,790 for a family of three). And they can’t wait years for their states to expand Medicaid. Thousands of them will die every year, just because they don’t have health insurance. If subsidies could be extended all the way down to 0% of poverty in states that haven’t expanded Medicaid, at least those people would have the possibility of having health insurance.
- Stagger open enrollment throughout the year. I wrote about this last spring, and I really feel like it would make the overall experience better for everyone. Carriers and exchanges could maintain level staffing throughout the year, allowing them to provide ongoing training and job security to their staff members. Hold times would be reasonable when you called a carrier or an exchange, and there wouldn’t be a mad rush to enroll millions of people in just three months each year. You could make open enrollment for everybody the month before their birthday for an effective date the first of their birthday month. You would also need to make the deductible start over on that effective date for everybody, instead of January 1st like they are now.
- Allow completely interoperable systems between carriers and exchanges, so that people could make changes to their plan by calling either the carrier or the exchange. I know that there are growing pains any time a new system is rolled out, but Jay has spent hundreds of hours on the phone this year with carriers and the exchange, often being told that the other entity has to be the one to fix whatever problem is at hand… and then being told the same thing by the other entity. I assume that the technology will become smoother and more interoperable as time goes on, but from a customer services perspective, this should be a priority.
That’s my top five. What would you fix or change about the healthcare reform law?